Prostate Artery Embolization (PAE)
What is Prostate Artery
Embolization (PAE)
Prostate Artery Embolization (PAE) is a cutting-edge, non-surgical treatment for men suffering from Benign Prostatic Hyperplasia (BPH)—also known as enlarged prostate. This minimally invasive procedure is performed by an interventional radiologist and provides effective relief from urinary symptoms without major surgery.
Prostate Artery Embolization is an outpatient procedure that reduces the prostate size by cutting off its blood supply. It is performed through a small puncture in the groin or wrist, and no incisions or general anesthesia are required.
Key benefits of PAE for BPH:
Some key benefits of the PAE procedure include:
- Safe, outpatient alternative to surgery
- Short recovery time
- Preserves sexual function
- High patient satisfaction and success rates
Is Prostate Artery Embolization Right for You?
This treatment is particularly well-suited for patients who meet one or more of the following criteria:
- You have frequent urination, weak urinary stream, or difficulty emptying your bladder
Have an enlarged prostate (typically greater than 50 grams)
Experience persistent BPH symptoms that have not improved with medication
Suffer from refractory hematuria (persistent blood in the urine)
Prefer to avoid surgical intervention
Are considered high-risk surgical candidates due to other medical conditions
Take anticoagulation (blood-thinning) medications
Use tobacco products, such as cigarettes
PAE offers a promising alternative for patients seeking symptom relief with reduced recovery time and fewer side effects compared to traditional surgical approaches.
Schedule Your Appointment Today
The PAE Procedure
Understanding how Prostate Artery Embolization (PAE) is performed is essential for patients considering this innovative treatment for enlarged prostate (BPH). Here’s a detailed look at what to expect before, during, and after the PAE procedure.
Before the Procedure
Before undergoing PAE, you’ll have a thorough evaluation by an interventional radiologist and urologist to confirm you are a good candidate for this minimally invasive BPH treatment.
Medical History & Physical Exam
- Your doctor will assess your urinary symptoms, medications, sexual health, and any other conditions like heart disease or diabetes.
- A pelvic CT angiogram or MRI is performed to map your prostate arteries, which can vary greatly between individuals.
- A transrectal ultrasound (TRUS) may be used to measure prostate size.
- Blood tests may be done to check your PSA level (Prostate-Specific Antigen) and to rule out infection or cancer.
- You’ll receive instructions on when to stop certain medications (e.g., blood thinners) and whether you need to fast before the procedure.
During the Procedure
The Prostate Artery Embolization procedure typically lasts 1 to 2 hours and is performed our very own outpatient surgical center located conveniently in Alpharetta, GA and Decatur, GA
- You’ll be given light sedation and local numbing at the catheter entry site—typically the femoral artery (groin) or radial artery (wrist).
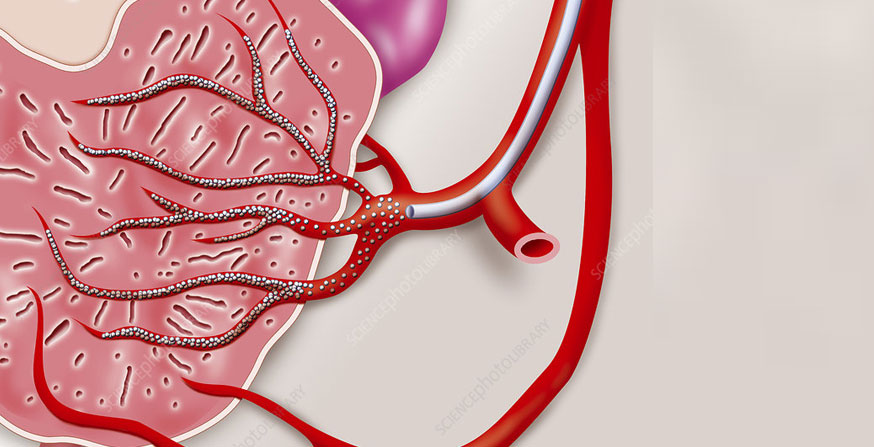
- A thin catheter is guided through your arteries using live X-ray (fluoroscopy). The radiologist carefully navigates to the small arteries that supply blood to the prostate.
- Tiny microspheres (embolic particles) are injected into the prostate arteries. These block blood flow to the prostate, causing it to shrink over time.
- The process is repeated on both sides of the prostate for complete treatment.
- After the procedure, you’ll be monitored for a short time to ensure stable vital signs and comfort before discharge.
After the Procedure
One of the major benefits of PAE for BPH is the quick and gentle recovery compared to traditional prostate surgeries.
- Patients return home within a few hours of the procedure
- You may experience urinary urgency or frequency, mild burning with urination, pelvic cramping or discomfort, or fatigue for a few days
- Pain relievers, antibiotics, or anti-inflammatory medications may be prescribed if needed
- Men typically report improvements in nighttime urination (nocturia), weak urinary stream, incomplete bladder emptying, urgency, and frequency. Follow up imaging or symptom assessments may be scheduled to ensure progress.
